Laser technology has been particularly revolutionary in medicine. Surgery is no longer the principal application of medical lasers, as their application in minimally invasive procedures has become quite prevalent. A variety of medical specialties have benefited from laser technology. This is remarkable considering that said technology has only been available for a relatively short period of time. Laser applications in medicine remain state-of-the-art. This notion is of singular importance as it reveals the pioneering nature of the technology and its advocates. It would seem that the future of this technology is limitless.
Laser technology has been particularly revolutionary in medicine. Surgery is no longer the principal application of medical lasers, as their application in minimally invasive procedures has become quite prevalent. A variety of medical specialties have benefited from laser technology. This is remarkable considering that said technology has only been available for a relatively short period of time. Laser applications in medicine remain state-of-the-art. This notion is of singular importance as it reveals the pioneering nature of the technology and its advocates. It would seem that the future of this technology is limitless.
 The laser beam
The laser beam
The laser beam and its components
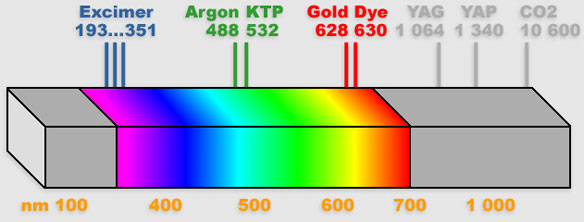
 Light constitutes only a small portion of the electromagnetic spectrum, including visible, ultraviolet and infrared light. Visible light, that which the retina senses, is an electromagnetic radiation with wavelengths ranging between 400 and 770 manometers. Despite being invisible to the naked eye, infrared and ultraviolet wavelengths are considered light. Taken separately, their wavelengths correspond to different colors ; blue corresponding to short wavelengths, and red to long wavelengths. White light results from the mix of all wavelengths within the visible spectrum.
Light constitutes only a small portion of the electromagnetic spectrum, including visible, ultraviolet and infrared light. Visible light, that which the retina senses, is an electromagnetic radiation with wavelengths ranging between 400 and 770 manometers. Despite being invisible to the naked eye, infrared and ultraviolet wavelengths are considered light. Taken separately, their wavelengths correspond to different colors ; blue corresponding to short wavelengths, and red to long wavelengths. White light results from the mix of all wavelengths within the visible spectrum.
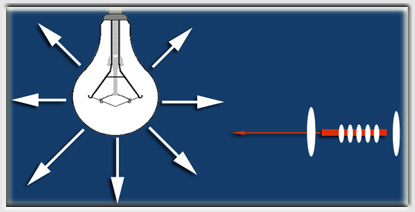
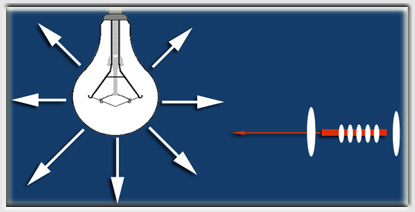 Conventional light sources, such as the incandescent lamp produce white light. This light results from heating a filament within the lightbulb. Each atom within the filament behaves as an isolated lamp emitting unsynchronized light in a 360-degree circle. Due to the random distribution in time, space and wavelength, the energy provided by the filament is dispersed.
Conventional light sources, such as the incandescent lamp produce white light. This light results from heating a filament within the lightbulb. Each atom within the filament behaves as an isolated lamp emitting unsynchronized light in a 360-degree circle. Due to the random distribution in time, space and wavelength, the energy provided by the filament is dispersed.
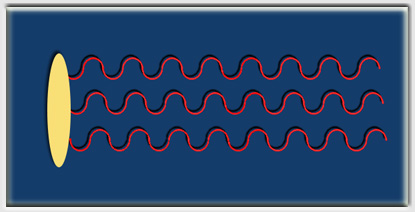
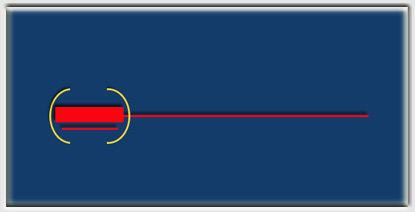
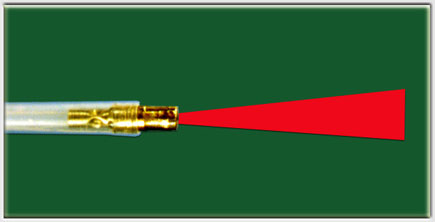
The laser beam is very different. The word laser is in fact an acronym for, « Light Amplification by Stimulated Emission of Radiation ». The stimulated source produces coherent light.
Laser beam characteristics
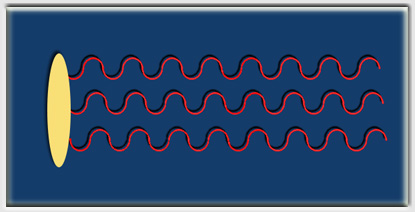 Lasers vary with respect to their biological effects, manipulation, and transmission. All lasers have coherence in common, collimation, and monochromatism. Coherence is defined as the distribution in phase of light waves in time and space. Collimation refers to the parallel emission of the light waves. Finally, mono chromatism refers to the uniformity of wavelength of the laser beam reflected in a single color.
Lasers vary with respect to their biological effects, manipulation, and transmission. All lasers have coherence in common, collimation, and monochromatism. Coherence is defined as the distribution in phase of light waves in time and space. Collimation refers to the parallel emission of the light waves. Finally, mono chromatism refers to the uniformity of wavelength of the laser beam reflected in a single color.
 Each of these characteristics corresponds to an advantage of lasers over conventional light sources. A laser’s power rests in its coherence. Laser light instead of becoming dispersed is distributed synergically, thus augmenting its effect upon impact. Collimation allows for long distance transmission without loss of power. The beam can be focused facilitating high-energy delivery to a specific target. Therefore, the power density at the point of impact is considerably superior to conventional light. Finally, mono-chromatism is, along with power settings and mode of distribution, responsible for the biological effect, insofar as varying wavelengths correspond to varying tissue effects.
Each of these characteristics corresponds to an advantage of lasers over conventional light sources. A laser’s power rests in its coherence. Laser light instead of becoming dispersed is distributed synergically, thus augmenting its effect upon impact. Collimation allows for long distance transmission without loss of power. The beam can be focused facilitating high-energy delivery to a specific target. Therefore, the power density at the point of impact is considerably superior to conventional light. Finally, mono-chromatism is, along with power settings and mode of distribution, responsible for the biological effect, insofar as varying wavelengths correspond to varying tissue effects.
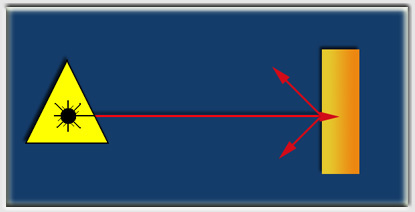
Creating a laser beam
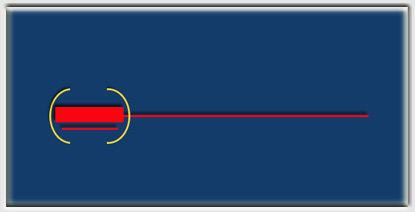 The basic components of a laser include the pump, the material to be activated and the pumping system. The chamber is a reflecting cavity, which presents a mirror on each extreme, of which one is semi-transparent. Stimulation of the laser beam source is variable and is achieved via an optical or electrical stimulus. The wavelength depends on the stimulated material. The mirrors guide the photons back to the source, thereby generating new photons of identical wavelength and orientation. The result of this stimulation is the laser beam.
The basic components of a laser include the pump, the material to be activated and the pumping system. The chamber is a reflecting cavity, which presents a mirror on each extreme, of which one is semi-transparent. Stimulation of the laser beam source is variable and is achieved via an optical or electrical stimulus. The wavelength depends on the stimulated material. The mirrors guide the photons back to the source, thereby generating new photons of identical wavelength and orientation. The result of this stimulation is the laser beam.
 Tissue interactions
Tissue interactions
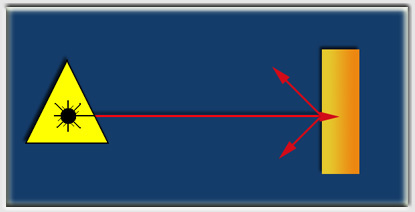 A variety of phenomena take place when the laser beam impacts upon the surface of living tissues. A part of the energy is reflected and the rest is absorbed. The relative importance of absorption versus reflection depends upon the wavelength and power used. Absorption can take place both at the surface or to a certain degree in depth.
A variety of phenomena take place when the laser beam impacts upon the surface of living tissues. A part of the energy is reflected and the rest is absorbed. The relative importance of absorption versus reflection depends upon the wavelength and power used. Absorption can take place both at the surface or to a certain degree in depth.
 Thermal effects
Thermal effects
The thermal effects of laser beams are the best understood and remain the cornerstone of therapy. Tissue effects depend in part on the temperature achieved. Necrosis and tissue inflammation are seen at temperatures below 40 degrees Celsius, whereas tissue vaporization can be seen at higher temperatures. To be exact, higher temperatures reflect greater absorption. The latter can be calculated by obtaining the product of power and length of exposure. The endoscopist must also keep in mind that the distance from the laser source to the target is also of crucial importance in determining laser tissue effects.
{{Power density}} at the target is inversely proportionate to the distance from the laser source. In addition, the volume of tissue treated is of great importance regarding biological effect.
_ {{Tissue penetration}} depends upon tissue type, its color, vascularity, and the wavelength employed. The effect of certain lasers, such as the YAG laser, relies in part on target tissue characteristics. This is illustrated in the following table.
 Tissue penetration in nm
Tissue penetration in nm
Table
| Laser |
nm |
Stomach |
Liver |
| CO2 |
10600 |
0.05 |
0.05 |
| Argon |
488 |
0.5 |
0.2 |
| YAGNd |
1060 |
2 |
0,8 |
This table clearly shows that tissue penetration of lasers such as the YAG is most pronounced if the tissue is white. The treatment strategy is based upon these considerations.
Medical lasers
Specificity of medical lasers
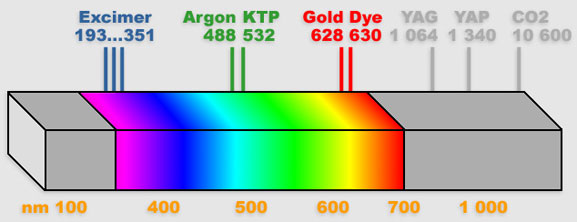
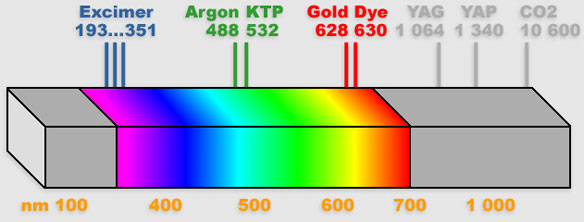
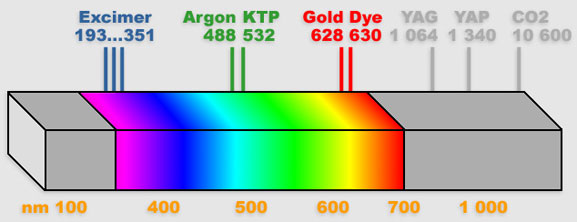 Laser tissue effect clearly depends on the type of laser used. A variety of these are available or currently in development, including ; the CO2, YAG, YAP, Argon, excimers, gold vapor, etc. Each laser has specific characteristics which make it unique depending on its power, wavelength, and mode of action.
Laser tissue effect clearly depends on the type of laser used. A variety of these are available or currently in development, including ; the CO2, YAG, YAP, Argon, excimers, gold vapor, etc. Each laser has specific characteristics which make it unique depending on its power, wavelength, and mode of action.
 Considering the complexity of human tissues, it is difficult to predict the biological effects of laser beams. The tissue color is very important. Melanin and hemoglobin, two of the principal human tissue pigments, absorb laser light differently. The interaction between tissue and laser depends in large part upon the relative importance of these two elements. Lasers, which emit infrared light, enjoy increased absorption causing moderate necrosis, and are therefore better suited for cutting than visible light lasers. They are most useful in precision resection.
Considering the complexity of human tissues, it is difficult to predict the biological effects of laser beams. The tissue color is very important. Melanin and hemoglobin, two of the principal human tissue pigments, absorb laser light differently. The interaction between tissue and laser depends in large part upon the relative importance of these two elements. Lasers, which emit infrared light, enjoy increased absorption causing moderate necrosis, and are therefore better suited for cutting than visible light lasers. They are most useful in precision resection.
Existing lasers
 CO2 lasers are commonly used in medicine. A monochromatic beam produced by the excitation of carbonic gas characterizes them. The invisible beam is absorbed by glass. Its wavelength is 10,600 nm (Infrared). Its power varies ranging from 20/30 watts to 40/60 watts. It causes primarily tissue vaporization. The CO2 laser is a precision instrument, which can be compared to a surgical scalpel. It can also have a weak coagulant effect. Unfortunately, the CO2 laser beam cannot be transmitted by a flexible fiber, thus limiting its use in endoscopy.
CO2 lasers are commonly used in medicine. A monochromatic beam produced by the excitation of carbonic gas characterizes them. The invisible beam is absorbed by glass. Its wavelength is 10,600 nm (Infrared). Its power varies ranging from 20/30 watts to 40/60 watts. It causes primarily tissue vaporization. The CO2 laser is a precision instrument, which can be compared to a surgical scalpel. It can also have a weak coagulant effect. Unfortunately, the CO2 laser beam cannot be transmitted by a flexible fiber, thus limiting its use in endoscopy.
 The argon laser was one of the first lasers to be used in medicine. Argon produces a visible laser beam in the green light spectrum with a wavelength of 488 nm (sometimes 514 nm). It can be transmitted via a flexible fiber, thus facilitating its use in endoscopy. Its power is moderate, around 3 watts. However, this does not imply a marginal tissue effect. Its biological effect is very different from that of CO2 lasers. Its salient characteristic is related to preferential absorption by red tissues. Adequate calibration can afford deep tissue effect without harming the tissue surface. Hence, it can be used to coagulate retinal blood vessels.
The argon laser was one of the first lasers to be used in medicine. Argon produces a visible laser beam in the green light spectrum with a wavelength of 488 nm (sometimes 514 nm). It can be transmitted via a flexible fiber, thus facilitating its use in endoscopy. Its power is moderate, around 3 watts. However, this does not imply a marginal tissue effect. Its biological effect is very different from that of CO2 lasers. Its salient characteristic is related to preferential absorption by red tissues. Adequate calibration can afford deep tissue effect without harming the tissue surface. Hence, it can be used to coagulate retinal blood vessels.
 YAG lasers have become particularly useful in endoscopy. They are invisible (infrared). Their wavelength is usually 1,064 nm, but may be doubled. Because the YAG laser beam can be transmitted via a flexible fiber, it is ideal for endoscopy. Power can reach 100 watts. It is important to understand the YAG laser’s tissue effects, as the overall effect can far exceed what is seen at the time of laser application by the endoscopist. The YAG laser beam is absorbed differently by tissues depending on color characteristics and power applied. A pale, poorly vascularized tissue is less vulnerable to its effects. The YAG laser is particularly versatile because it can be employed either to coagulate or vaporize tissues.
YAG lasers have become particularly useful in endoscopy. They are invisible (infrared). Their wavelength is usually 1,064 nm, but may be doubled. Because the YAG laser beam can be transmitted via a flexible fiber, it is ideal for endoscopy. Power can reach 100 watts. It is important to understand the YAG laser’s tissue effects, as the overall effect can far exceed what is seen at the time of laser application by the endoscopist. The YAG laser beam is absorbed differently by tissues depending on color characteristics and power applied. A pale, poorly vascularized tissue is less vulnerable to its effects. The YAG laser is particularly versatile because it can be employed either to coagulate or vaporize tissues.
 The YAP (Yttrium Aluminium Pevroskite) laser has a wavelength of 1340 nm corresponding with improved tissue absorption. It is ideal for coagulation, making it quite valuable in bronchology.
The YAP (Yttrium Aluminium Pevroskite) laser has a wavelength of 1340 nm corresponding with improved tissue absorption. It is ideal for coagulation, making it quite valuable in bronchology.
 Metallic vapor lasers are seldom used. The most common among these are gold, copper, manganese, and barium. Copper lasers have wavelengths ranging between 511 nm and 578 nm, green and yellow. Gold vapor lasers enjoy a wavelength in the infrared spectrum (311 nm), but can also be bright red (628 nm). Lead lasers have a wavelength of 723 nm (red), and barium is in the ultraviolet spectrum at 1500 nm. Tissue effect, as mentioned earlier, depends on the wavelength chosen.
Metallic vapor lasers are seldom used. The most common among these are gold, copper, manganese, and barium. Copper lasers have wavelengths ranging between 511 nm and 578 nm, green and yellow. Gold vapor lasers enjoy a wavelength in the infrared spectrum (311 nm), but can also be bright red (628 nm). Lead lasers have a wavelength of 723 nm (red), and barium is in the ultraviolet spectrum at 1500 nm. Tissue effect, as mentioned earlier, depends on the wavelength chosen.
Recently developed excimer lasers employ rare gases as the source. Their biologic effect appears to reflect local tissue destruction by mechanical means. These lasers are quite promising in the treatment of atheromatous plaques. Available wavelengths are variable, 193, 249, 308, 351 nm, depending on the gas used.
 Dye lasers enjoy different wavelengths depending on the dye used. They range between 360 to 700 nm, thus encompassing the entire visible spectrum. Dye lasers require the use of a second laser, which will cause excitation by optical pumping. The latter is usually a Krypton, Argon, or metallic vapor laser. They are used primarily in detecting abnormal tissue fluorescence (630 nm), and tumor destruction (405 nm) in conjunction with hematoporphyrin derivatives.
Dye lasers enjoy different wavelengths depending on the dye used. They range between 360 to 700 nm, thus encompassing the entire visible spectrum. Dye lasers require the use of a second laser, which will cause excitation by optical pumping. The latter is usually a Krypton, Argon, or metallic vapor laser. They are used primarily in detecting abnormal tissue fluorescence (630 nm), and tumor destruction (405 nm) in conjunction with hematoporphyrin derivatives.
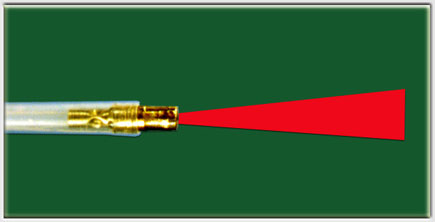
Advantages of the YAG and YAP lasers in endoscopic resection
 The YAG and YAP lasers are most suitable for use in endoscopy for a variety of reasons. One advantage is their ability to provide simultaneous precision cutting and hemostasis. Because they can be transmitted by a flexible fiber, they can deliver undiluted power at the extremity of the bronchoscope. Anywhere between 10 to 100 watts can be delivered using a fiber with a 2.4 mm diameter. The fibers are generally 4 meters long, but can be longer if desired. A continuous jet of cold air-cools the fiber during treatment.
The YAG and YAP lasers are most suitable for use in endoscopy for a variety of reasons. One advantage is their ability to provide simultaneous precision cutting and hemostasis. Because they can be transmitted by a flexible fiber, they can deliver undiluted power at the extremity of the bronchoscope. Anywhere between 10 to 100 watts can be delivered using a fiber with a 2.4 mm diameter. The fibers are generally 4 meters long, but can be longer if desired. A continuous jet of cold air-cools the fiber during treatment.
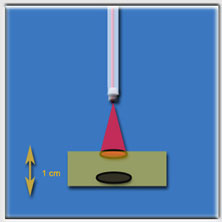
The biologic effects of these near-infrared lasers are far superior to those seen with the naked eye. The key variables determining tissue effect are : power, distance from the target, tissue coloration, and the duration and frequency of laser firing.
 Tissue vaporization is most likely to occur when utilizing high power density on dark tissues.
Tissue vaporization is most likely to occur when utilizing high power density on dark tissues.
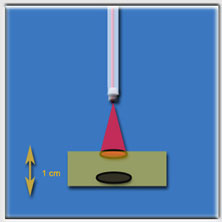
Power density in a laser is inversely proportionate to the distance from the target, and directly proportionate to the power used.
Once tissue destruction takes place, the target becomes charred and local absorption of all the laser’s energy occurs at the surface, resulting in more pronounced vaporization.
This limits tissue penetration by the laser’s energy, but may lead to ulceration at the target site of several millimeters.
 Tissue retraction is most commonly seen with moderate power settings while targeting pale tissues. While this tissue effect precludes direct photocoagulation, it is possible to diminish tissue vascularization as a result of tissue retraction, leading indirectly to hemostasis. Tissue penetration is achieved in this way without tissue destruction. It is not always easy to choose between tissue retraction and vaporization.
Tissue retraction is most commonly seen with moderate power settings while targeting pale tissues. While this tissue effect precludes direct photocoagulation, it is possible to diminish tissue vascularization as a result of tissue retraction, leading indirectly to hemostasis. Tissue penetration is achieved in this way without tissue destruction. It is not always easy to choose between tissue retraction and vaporization.
Laser power density may be controlled by changing the laser’s power settings or by distancing the extremity of the laser fiber from the target. In endoscopy, it is often more expedient to retract the laser fiber, thus reducing power density delivered to the target rather than altering the power settings.
 Collateral tissue effects depend on the color of surrounding tissues, power density, and the angle of attack. This is a fundamental notion worth dwelling on. Every endoscopist employing a YAG or YAP laser should be aware of two important risks of the procedure. When the laser beam is fired on pale tissue using moderate power settings, the laser seems to have little if any surface effect while its energy is absorbed several millimeters deep. This effect is unpredictable and may lead to perforation beyond the surface of the target. This dreadful complication has been well described in the rectum following laser treatment of bladder lesions.
Collateral tissue effects depend on the color of surrounding tissues, power density, and the angle of attack. This is a fundamental notion worth dwelling on. Every endoscopist employing a YAG or YAP laser should be aware of two important risks of the procedure. When the laser beam is fired on pale tissue using moderate power settings, the laser seems to have little if any surface effect while its energy is absorbed several millimeters deep. This effect is unpredictable and may lead to perforation beyond the surface of the target. This dreadful complication has been well described in the rectum following laser treatment of bladder lesions.
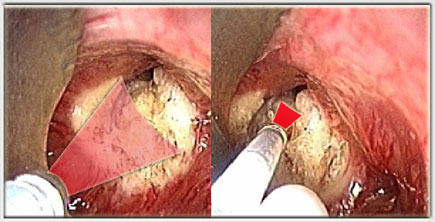
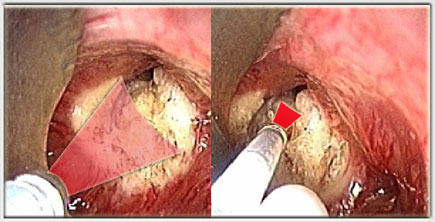
 The endoscopist should be particularly aware of another feared complication of laser treatment described by Jack Fisher ; the so-called popcorn effect.
The endoscopist should be particularly aware of another feared complication of laser treatment described by Jack Fisher ; the so-called popcorn effect.
If living tissue is irradiated for a prolonged period of time (as brief as 10-15 seconds) without changing the point of impact, the tissue has no time to dissipate the heat generated by the laser. This can lead to vapor accumulation and eventually an explosion.
Firing a laser fiber 4-mm away from rat liver for 16 seconds employing 40 watts of power, we have experimentally demonstrated this effect. It is one of the reasons why we prefer using the discontinuous YAG laser mode.
 We believe the advantages of this type of laser treatment outweigh the disadvantages. For this reason we recommend the use of YAG and YAP lasers in tracheobronchial endoscopic applications.
We believe the advantages of this type of laser treatment outweigh the disadvantages. For this reason we recommend the use of YAG and YAP lasers in tracheobronchial endoscopic applications.
In particular, we find the devascularization effect along with the probable antiviral effect of the laser on papillomas quite advantageous, while remaining keenly aware of the risk of cartilaginous injury in the treatment of tracheal stenosis and the ¨popcorn¨ effect as definite disadvantages.
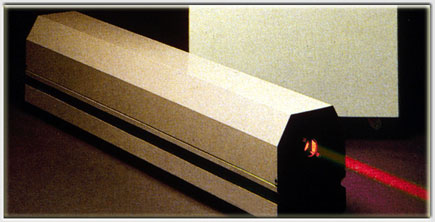
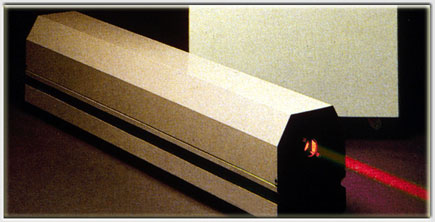
The medical application of YAG and YAP lasers
 A number of YAG lasers are currently available presenting similar design characteristics. All of them are subject to strict regulation in terms of safety and reliability and therefore quite expensive. Aside from safety concerns regarding the electrical system and laser fiber cooling, they are all carefully designed in order to avoid dispersal of the laser beam, both at the level of the apparatus itself and its connections, as well as that of its detachable parts. For example, the laser pedal has been designed to preclude inadvertent firing of the laser. An emergency button capable of stopping the laser from firing is also available and quite accessible in case it is needed.
A number of YAG lasers are currently available presenting similar design characteristics. All of them are subject to strict regulation in terms of safety and reliability and therefore quite expensive. Aside from safety concerns regarding the electrical system and laser fiber cooling, they are all carefully designed in order to avoid dispersal of the laser beam, both at the level of the apparatus itself and its connections, as well as that of its detachable parts. For example, the laser pedal has been designed to preclude inadvertent firing of the laser. An emergency button capable of stopping the laser from firing is also available and quite accessible in case it is needed.
 In order to avoid retinal damage, goggles specific to the YAG or YAP laser wavelengths must be worn by all personnel.
In order to avoid retinal damage, goggles specific to the YAG or YAP laser wavelengths must be worn by all personnel.
The quality of these goggles is of the utmost importance in order to facilitate precision treatment and adequate visualization.
 The fiberoptic equipment must also be top notch. Given their elevated price, one must demand good quality, particularly in the design of the cooling system.
The fiberoptic equipment must also be top notch. Given their elevated price, one must demand good quality, particularly in the design of the cooling system.
Four meters should be the minimum length, but we recommend 6 meter long fibers.
 Standard fibers are generally 2.6 mm in diameter or 1 mm in case they are unsheathed.
Standard fibers are generally 2.6 mm in diameter or 1 mm in case they are unsheathed.
However, smaller fibers are available ranging between 200 to 600 microns.
The latter are useful in pediatric cases.
 Both YAG and YAP lasers are invisible and therefore require a guiding laser beam for targeting.
Both YAG and YAP lasers are invisible and therefore require a guiding laser beam for targeting.
The helium neon laser is commonly used for this purpose.
Paradoxically enough, its red color is easily identified despite targeting tissues of the same color.
Green, yellow, or white guiding lasers are also available, some of which can be modified on demand.
 Most modern medical lasers are computerized allowing for precise control over time of impact, laser power settings, and mode of action. Because most of these lasers are employed in a variety of medical specialties, the ideal instrument should be able to generate anywhere from a few watts to 100 watts of power. It should be capable of switching back and forth from continuous mode to discontinuous mode in less than one second, and when fired in discontinuous mode, the laser should be able to fire repeatedly without having to lift the foot from the pedal each time.
Most modern medical lasers are computerized allowing for precise control over time of impact, laser power settings, and mode of action. Because most of these lasers are employed in a variety of medical specialties, the ideal instrument should be able to generate anywhere from a few watts to 100 watts of power. It should be capable of switching back and forth from continuous mode to discontinuous mode in less than one second, and when fired in discontinuous mode, the laser should be able to fire repeatedly without having to lift the foot from the pedal each time.
The choice of laser depends essentially upon a variety of criteria, including the quality of long-term servicing of the instrument by the manufacturer, as well as the quality and price of all of its accessories, especially the laser fiber.