|
Index >
Technique > Endoscopic assessment |
Endoscopic assessment |
|
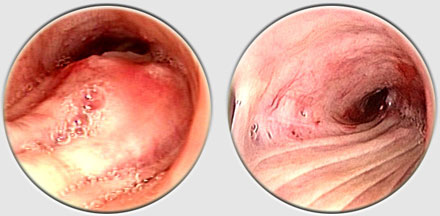
The endoscopist should note the appearance of any lesions, their intrinsic or extrinsic nature, and their location with respect to the carina, vocal cords, etc. The degree of obstruction should be noted in terms of airway patency, and length of involvement as well as the presence or absence of distal secretions. Assessing the apparent vascularity of a tumor is also important because it might help determine the therapeutic approach to a given lesion. In these cases, sampling should be postponed until rigid bronchoscopy can be performed. Multiple, large specimens are necessary to ensure accurate histologic diagnosis of most lesions. Brush specimens for cytology are not as reliable as biopsy samples. Most lesions can be classified as inflammatory or tumoral. Inflammatory lesions often lead to tracheal stenosis and may be associated with respiratory compromise. |
|
move
up
|
move
down
|
|
previous
|
next |